Issues
Complex / high energy injuries
Management of soft tissues critical / staged treatment
Restoration of alignment & joint surface imperative
Outcome guarded - high incidence of OA and complications
Outcomes
- 1 year outcome of 91 plafond injuries
- 57% return to work at 1 year
- 27% reported residual moderate to severe pain
- 80 patients at a mean of 3.2 years post injury
- 35% reported ongoing stiffness and pain
- 43% not working
Epidemiology
5 - 7% of tibia fractures
35 - 40 years
Males 3 x
Etiology
Rapid axial load of talus into tibia
Very high energy
Anatomy
Soft tissues very poor especially over anteromedial tibia
- thin skin
- absence of muscle and adipose tissue
- lack of deep veins
OTA Classfication
43-A Extra Articular
43-B Partial Articular
43-C Complete Articular
Management
Staged treatment - External Fixation followed by delayed fixation
Management of the soft tissues is the key to a good outcome
Spanning external fixation
- holds out length
- helps soft tissues recover
- wait until swelling down
- wrinkled skin, blisters resolved
- wait 3 weeks plus if needed
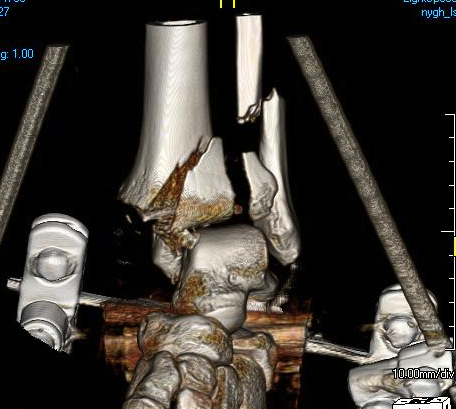
Technique of ankle bridging delta frame
- two pins in the tibia away from surgical site
- transcalcaneal threaded pin placed medial to lateral
- pin in base of first metatarsal to keep foot in neutral position and prevent equinus contracture
- note: pin in base of first metatarsal places deep plantar branch of dorsalis pedis at risk
+/- fibular fixation
- can keep fracture out to length / maintain reduction
- must avoid fibula malreduction as makes later tibial ORIF very difficult
- must consider future incisions
- should only be done by definitive surgeon
- best through posterolateral approach
CT after external fixation application
AO foundation surgical technique
Vumedi bridging external fixation video






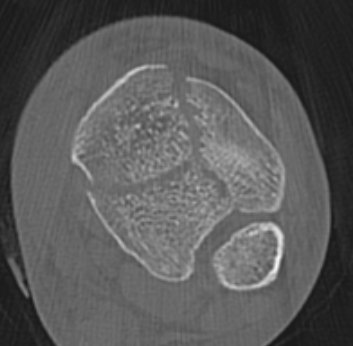
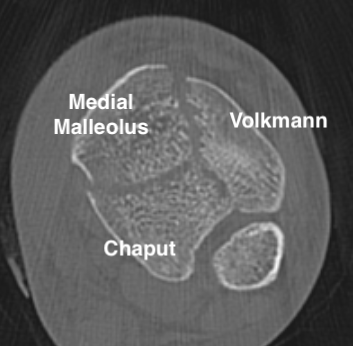
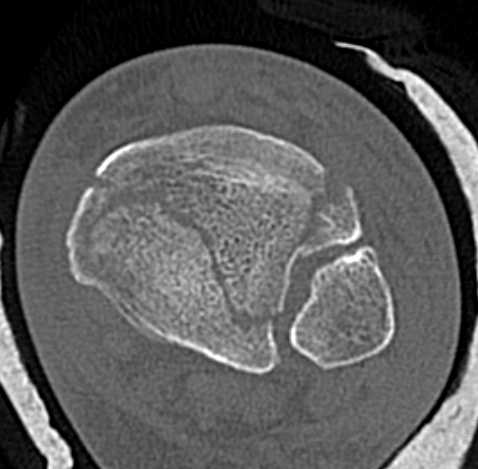
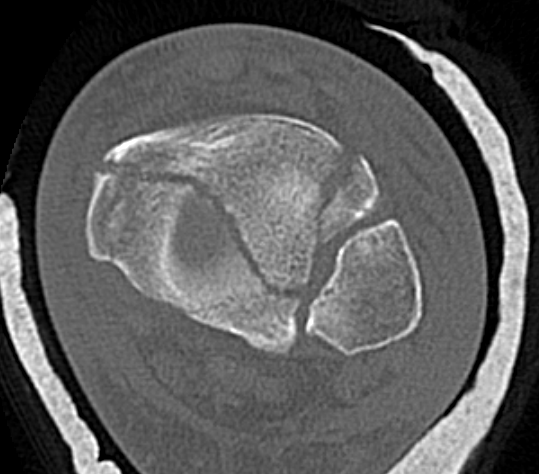
CT scan
Commonly 3 fracture configurations
- medial malleolus
- posterolateral fragment / Volkmann
- anterolateral fragment / Chaput

Associated injuries
Compound wounds
- 14 open tibial plafond fractures
- 28% deep infection
- 43% delayed union
Fibula fractures


Bonnevialle et al. Orthop Traumatol Surg Res 2010
- may aid reduction if able to anatomically reduce the fibula
- however, may contribute to nonunion
- if fibular fracture is malreduced, can contribute to tibial malreduction and malunion
Gallimore et al J Foot Ankle Surg 2024
- meta-analysis of fibular fixation versus no fixation in tibial plafond
- 4 studies
- no difference in incidence of nonunion / malunion
Syndesmotic / Syndesmotic equivalent injuries

Haller et al. J Orthop Trauma 2019
- 14/735 (2%) had missed syndesmotic injuries
- 93% of these patients developed post traumatic osteoarthritis
- syndesmotic equivalent injuries more common with Chaput (AITFL Ligament) / Volkmann fragments (PITFL) or fibular avulsion
Surgical options
ORIF with plates
Limited internal fixation + external fixation
IM nail
Primary fusion
ORIF versus external fixation
Malik-Tabassum et al. Injury 2020
- meta-analysis of ORIF v circular external fixation
- increased rate of hardware removal for ORIF
- reduced rate of osteoarthritis with ORIF
- no difference in superficial or deep injection, or secondary fusion
- no obvious difference in outcomes
- more severe injuries tended to be treated with circular external fixation
IM nail
Beytumar et al Acta Orthop Traumatol Turc 2017
- comparison of IMN versus plate for simple intra-articular pilon
- increased valgus malunion and recurvatum with nail
Primary arthrodesis
- comminuted un-reconstructable pilon fractures
- anterior plate fusion in 12 ankles
- 9/12 required external fixation for metaphyseal fracture
- healed at 4 months with 88% good or excellent result
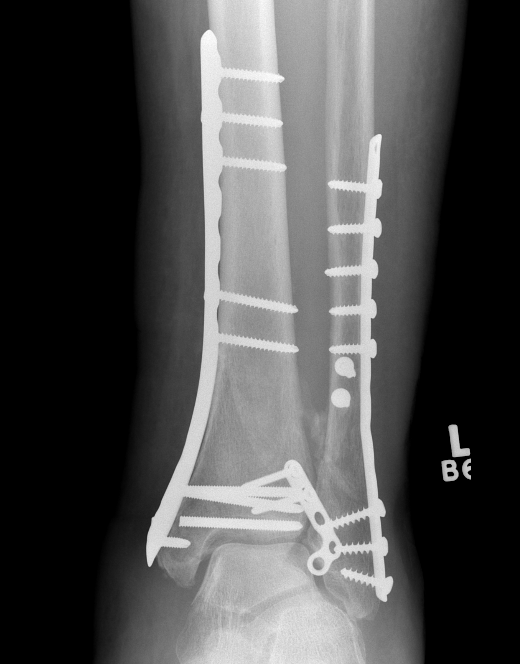
ORIF with Plates
Principle
Restore articular surface
Fix articular surface to metaphysis
Techniques to minimize complications
Long delays until definitive surgical treatment using initial spanning external fixation
The use of small, low-profile, anatomical implants
Avoidance of incisions over the anteromedial tibia
All incisions 7 cm apart
The use of indirect reduction techniques minimizing soft tissue stripping / MIPO
Careful surgical management of the soft tissues at all times
Surgical Approaches
1. Anteromedial - between tibialis anterior and saphenous nerve / vein
2. Anterior - between tibialis anterior and EHL
3. Anterolateral - between fibula and peroneus tertius
4. Posteromedial - between FHL and NV bundle
5. Posterolateral - between peroneal tendons and FHL
Vumedi surgical approaches for Pilon fractures
Anatomical Plates


Synthes medial plate Synthes anterolateral plate
Anterolateral / anterocentral approach
Indication
- anterolateral / Chaput fragment
- valgus configuration
- anterolateral plate
Issue
- will not stabilize medial fragments
- need separate incision
Incision
- anterocentral: centered on ankle joint
- anterolateral: in line with 4th metatarsal
- preserve branches superficial peroneal nerve
- divide extensor retinaculum
- anterolateral: all extensor tendons reflected medially, including peroneus tertius
- anterocentral: between tibialis anterior and EHL








Anteromedial approach
Indication
- large medial fragment
- varus configuation
- anteromedial plate
Issue
- skin and soft tissues poor
- increased risk of wound complication
- use MIPO techniques
Technique
- medial to tibialis anterior
- extensor compartment retracted laterally
- can make small anterolateral incision to fix small Chaput fracture











Posterolateral approach
Indication
- large posterior tibial fragment requiring buttress
Technique
- patient lateral decubitus or prone
- incision halfway between tendoachilles and fibular
- approach to posterior tibia: between peroneals and FHL
- approach to fibular: anterior to peroneal tendons
Surgical Technique
AO surgery reference technique
Position
- supine on radiolucent table
- IV antibiotics
- tourniquet for 2 hours then release
Consider fibula ORIF
- holds fracture out to length
- via posterolateral incision
- need wide skin bridge from anterior incision
- must avoid malreduction
Anatomical reduction joint surface
- open fracture site / open joint / washout haematoma
- can apply femoral distractor to view joint surface
- 4 mm Shanz pins in talar neck laterally, and into tibia proximal to plate
- examine talar dome using periosteal elevator
- ORIF small osteochondral fragments with small modular screws (1.5 - 2 mm)
Attach metaphysis to diaphysis
- anatomically contoured low profile locking plates
- anterolateral L shaped plate via anterior wound
- small incisions proximally to insert screws
- 8 cortices above fracture
- small medial incision to insert medial plate percutaneously / MIPO techniques
Limited Internal Fixation + External fixation
Indications
Poor skin
Multiple co-morbidities
High risk of wound complications






Technique
Limited internal fixation
- anterior approach
- reduction and fixation of joint line
Hybrid external fixation
- HA coated Schanz pins in proximal tibia
- +/- calcaneal pins
- +/- olive K wires in distal tibia
Results
- systematic review of circular external fixation for tibial plafond
- 303 patients
- mean time to union 21 weeks
- malunion in 12%
- 54% pin site infections, 5% deep infection
- 33% excellent functional outcomes
Wang et al J Foot Ankle Surg 2015
- systematic review of ORIF versus external fixation + limited internal fixation
- 500 fractures
- no difference in complications / union rates / outcomes
Complications
Wound breakdown

Deep infection
Bullock et al J Orthop Trauma 2022
- systematic review of Type C plafond fractures
- 9% rate of deep infection
Shafiq et al J Orthop Trauma 2023
- 175 pilon fractures
- increased risk of infection with surgical time > 120 minutes
- increased risk of infection with fibular plating
Stiffness
Osteoarthritis
Harris et al. Foot Ankle Int 2006
- 79 pilon fractures with mean follow up 2 years
- 40% developed post traumatic arthritis
Malunion




Nonunion
Haller et al. J Orthop Trauma 2019
- incidence of nonunion 14% (72/518)
- associated with open fractures, bone loss, and smoking
